
E/M vs. Eye Codes: How to Choose? Part 2 of 3

This latest installment of our three-part series comparing the E/M and the eye codes focuses on the latter, reviewing their definitions, examination requirements and ambiguities. The eye codes are technically referred to in CPT as General Ophthalmological Services. Most providers have never really studied these codes — they have just always used them, not even being aware that they are a part of CPT or that there are rules for them.
There are four codes: two “new patient” codes for new intermediate and comprehensive services and two “established patient” codes for the same services (92002, 92004, 92012, 92014). There are both national and local requirements for these codes: the national requirements being found in CPT (Current Procedural Terminology) and the local requirements being found in your Medicare contractor's LCD (Local Coverage Determination). Most LCDs include the CPT definitions. Be sure you look up your Medicare carrier's policy — many ophthalmologists don't even know there are such things. You are responsible for adhering to them. The codes as listed in CPT are as follows.
92002 Ophthalmological services: medical examination and evaluation with initiation of diagnostic and treatment program; intermediate, new patient
92004 Ophthalmological services: medical examination and evaluation with initiation of diagnostic and treatment program; comprehensive, new patient, one or more visits
92012 Ophthalmological services: medical examination and evaluation, with initiation or continuation of diagnostic and treatment program; intermediate, established patient
92014 Ophthalmological services: medical examination and evaluation, with initiation or continuation of diagnostic and treatment program; comprehensive, established patient, one or more visits
Many providers are not aware of the narrative descriptions in CPT until they find themselves in an audit situation. These are found at the back of the CPT book, under Special Ophthalmological Services.
The descriptions for the intermediate eye codes are as follows: “Intermediate ophthalmological services describes an evaluation of a new or existing condition complicated with a new diagnostic or management problem not necessarily relating to the primary diagnosis, including history, general medical observation, external ocular and adnexal examination and other diagnostic procedures as indicated; may include the use of mydriasis for ophthalmoscopy.”
The descriptions for the comprehensive eye codes contain the following excerpted information:
“Comprehensive ophthalmological services describes a general evaluation of the complete visual system. The comprehensive services constitute a single service entity but need not be performed at one session. The service includes history, general medical observation, external and ophthalmoscopic examination, gross visual fields and basic sensorimotor examination. It often includes, as indicated: biomicroscopy, examination with cycloplegia or mydriasis and tonometry. It always includes initiation of diagnostic and treatment programs.
Intermediate and comprehensive ophthalmological services constitute integrated services in which medical decision-making cannot be separated from the examining techniques used. Itemization of service components, such as slit lamp examination, keratometry, routine ophthalmoscopy, retinos copy, tonometry, or motor evaluation is not applicable.
Initiation of diagnostic and treatment program includes the prescription of medication, and arranging for special ophthalmological diagnostic or treatment services, consultations, laboratory procedures and radiological services.
Special ophthalmological services describes services in which a special evaluation of part of the visual system is made, which goes beyond the services included under general ophthalmological services, or in which special treatment is given. Special ophthalmological services may be reported in addition to the general ophthalmological services or evaluation and management services.”
A significant problem with the eye codes is that the definitions in the general description of the codes do not correspond with the code descriptors found next to the CPT code numbers. In both set of codes for established patients, the code descriptor allows for “initiation or continuation of diagnostic and treatment programs.”
However, in the narrative for the comprehensive codes there is a statement that the code “always includes initiation of diagnostic and treatment programs.” In my experience, this should be adhered to when using 92004 and 92014 because under audit the code will be disallowed or down-coded if that does not occur.
I think it is acceptable to use 92012 for continuation of medical treatment, such as in glaucoma follow ups.
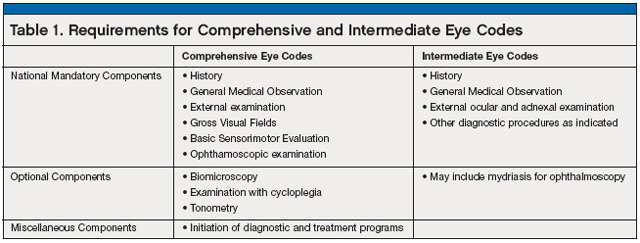
The intermediate eye exam codes require an external ocular and adnexal examination, whereas the comprehensive examination additionally requires gross visual fields, basic sensorimotor evaluation and an ophthalmoscopic examination.
And in many states Medicare contractors have mandated elements similar, but not identical, to those found in the E/M codes. A typical policy may list 10 elements and state that, in order to bill an intermediate service, fewer than seven elements would be performed and documented, and that more than eight should be performed and documented for a comprehensive examination. The number of elements themselves and the number required for each category vary from carrier to carrier.
Most of the LCD policies state that practices should use E/M codes for “minimal services.” A minimal service is a very brief examination, such as follow-up for a corneal abrasion or conjunctivitis. The service typically includes one to three elements and should be billed with code 99212.
Dilation requirements differ for each Medicare contractor wherein some carriers mandate that the pupils be dilated in order to count the posterior segment elements and others do not. Table 1 outlines the exam requirements for comprehensive and intermediate eye codes.
When Medicare audits ophthalmic services and procedures, denials for services are most often based on lack of medical necessity. Medicare states that all services must be medically necessary and medically reasonable — and this broad concept gives them a lot of leeway in interpreting your coding, chart documentation, and their decisions for audit and payment. It is not a matter of what a physician deems is “good medicine” or medically appropriate. Rather, the service must be warranted in Medicare's opinion.
When dealing with E/M services or general ophthalmological services, not only does the service itself have to be medically necessary — so do the elements within the service such as confrontation fields and sensorimotor evaluation. As an example, in a patient being followed for glaucoma with automated visual fields, there would be no medical necessity for confrontation fields. In a patient with a unilateral choroidal nevus, there would be no medical necessity to perform extended ophthalmoscopy in the other eye in the absence of symptoms.
Several years ago, audits of the comprehensive eye codes (92004/92014) began, with resultant downcoding of claims based on the lack of initiation of a diagnostic or treatment program. These codes should meet the mandate of always including initiation of diagnostic and treatment programs that are defined as including “the prescription of medication, and arranging for special diagnostic or treatment services, consultations, laboratory procedures and radiological services.” The program does not have to be a reimbursable service; prescribing eyeglasses would count. Ordering of any of the special ophthalmic diagnostic tests, such as visual fields or OCT, is considered as initiating a diagnostic program. An order such as “Return PRN” or “Return to Clinic in one year” would not be an initiation of a diagnostic or treatment program, nor would “Continue same meds.”
In part 3 of this series, we will review how to make the choice between E/M and eye codes based on compliance and reimbursement optimization. Remember: under audit, your best defense is a good chart documentation offense! OM
| Riva Lee Asbell can be contacted at www.rivaleeasbell.com, where the order form for her new book, Tips on Ophthalmic Surgical Coding by Subspecialty, can be found and downloaded under Products/Books. |